An Essential Guide to Complex Trauma
A guide to complex trauma that goes beyond textbook definitions

I’ve put this complex trauma guide together to help those with lived experiences. Up until recently, complex trauma has not been recognised by a diagnosis and only acknowledged by some in the professional community. As a diagnosis has only existed since 2022, and it still remains absent in the mainstream diagnostic manual, it continues to be a confusing area. I’m going to make sense of complex trauma, as distinct from general trauma, so hopefully you can understand where you fit in. I write about complex trauma from my professional experience and advanced training, so I hope to give you a perspective that you won’t find in all the general information on the web . Finally, I’ll explore the journey of trauma recovery—yes, it’s possible!—and offer tips on finding the right therapy, so you won’t waste years on ineffective treatments.
Complex trauma, complex post traumatic stress disorder, post traumatic stress disorder, borderline personality disorder? What do you have?! Not even the professionals can agree.
The historical context of trauma in mental health shows how complex trauma eventually becomes seen as a distinct entity, highlighting the evolution of diagnosis and treatment approaches in the field.
1.0 A very brief history of the trauma field
Until recently, the mental health field, particularly within the trauma domain, has primarily concentrated on individuals impacted by single incident traumas. These include experiences like surviving a serious car accident, enduring a bushfire, or being a victim of burglary—events that occur as isolated incidents.
Post Traumatic Stress Disorder (PTSD) has been the primary diagnosis for individuals grappling with the aftermath of such events. This diagnosis applies to those who have faced one-off traumas and meet the qualifying criteria of ‘exposure to an actual or threatened death, serious injury, or sexual violence’.
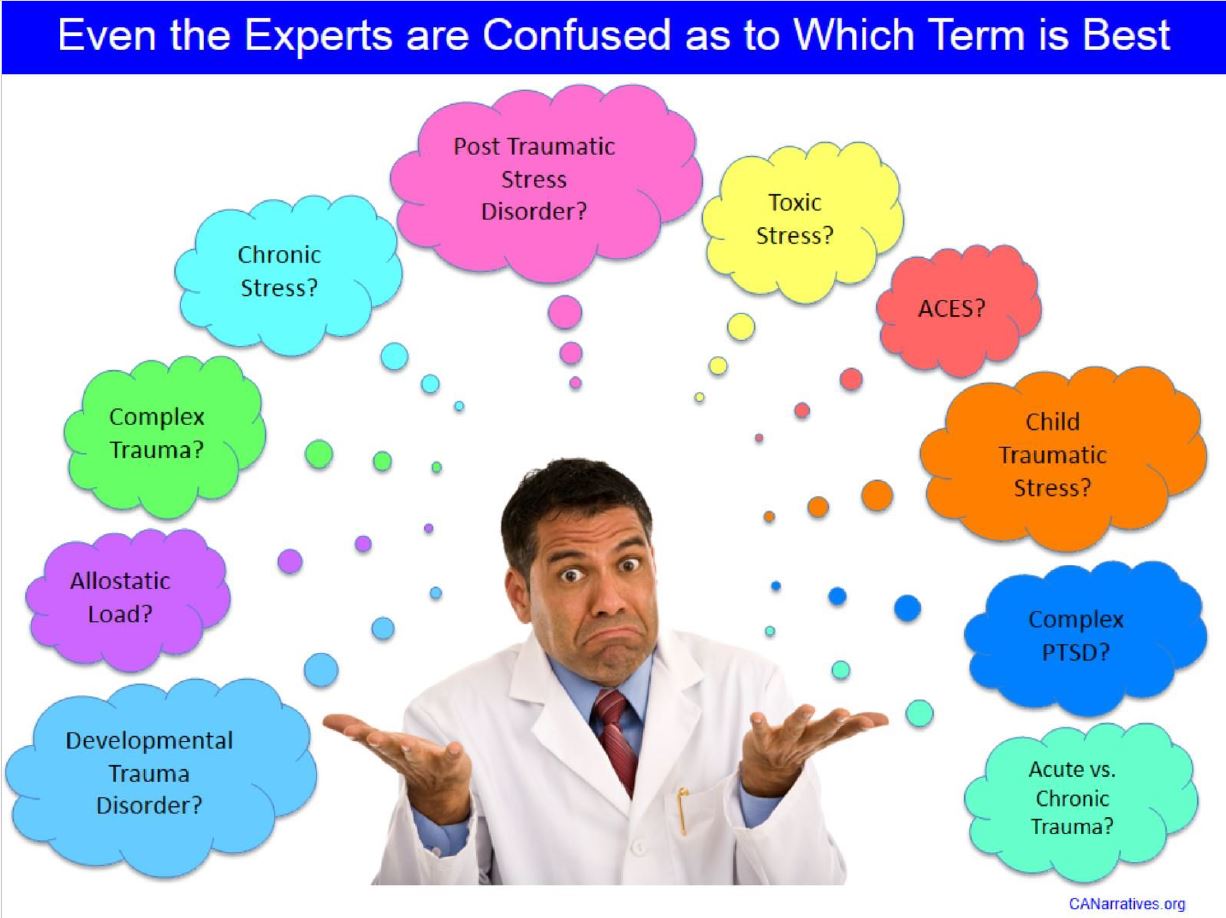
Image source: Childhood Adversity Narratives
Complex Trauma, can occur when someone is exposed to prolonged and repetitive adversity, such as experiences like child abuse or family violence. This type of trauma has been unrecognised by the mental health field until recently. Unlike single incident traumas, these traumas unfold over extended periods, sometimes spanning years. People who have endured trauma like this may not have faced immediate threats of death or injury, but the psychological impact they bear is profound. However, up until recently, there has not been a relevant diagnosis for them, and they have been precluded from a diagnosis of PTSD because they often don’t meet the qualifying criteria ‘exposure to an actual or threatened death, serious injury, or sexual violence’.
INFO
The DSM 5 (The Diagnostic and Statistical Manual of Mental Disorders, 5th edition) is a universal book used by mental health clinicians and researchers, for clinical diagnosis and treatment planning of mental health conditions.
The ICD 11 (The International Classification of Diseases, 11th Revision) is published by the World Health Organisation, and is a global standard for classifying diseases and health conditions, including physical and mental disorders. It’s used for medical billing, statistical tracking, and epidemiological research.
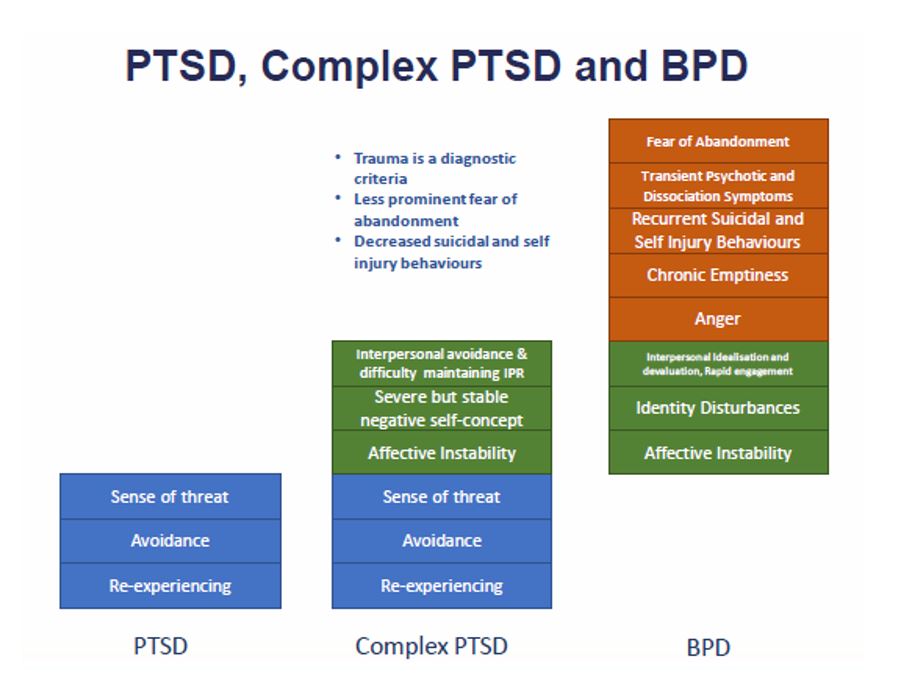
Image source: BPD Foundation
This diagram shows the overlap between three of the main trauma disorders.
“In 2009, Bessel van der Kolk underlined the anomaly that what is widely called complex trauma officially did ‘not exist’. This was despite the ‘vast amounts of knowledge’ in relation to it, and that it possibly comprised ‘the most common set of psychological problems to drive human beings into psychiatric care’.” Blue Knot, (2019)
1.1 Some diagnostic recognition for complex trauma survivors
In January 2022, the ICD 11 officially recognised Complex Post Traumatic Stress Disorder (CPTSD) as a diagnosis, marking a significant step forward in acknowledging the complexities of trauma. While Complex PTSD offers some recognition of the multifaceted nature of complex trauma, it does not encompass its full scope. Notably, complex trauma and Complex PTSD are not currently recognised with a diagnosis in the DSM 5.
1.2 Why the Previous Diagnoses Failed Complex Trauma Survivors
Until the inclusion of Complex PTSD in the ICD 11 (2022), complex trauma survivors were either not recognised by a diagnosis or slotted in to a ill-fitting, but close enough, diagnosis. These included –
Post Traumatic Stress Disorder (you can read more about PTSD, and why it wasn’t a great fit here).
Borderline Personality Disorder (read more about the overlap with Complex PTSD and PTSD here).
Although the DSM 5’s 2013 edition included a ‘dissociative subtype’ of PTSD, aimed at capturing some of the effects of complex trauma, it still falls short of fully acknowledging its comprehensive impacts.
As we delve into the understanding of psychological trauma and its implications, it’s important to recognise the recent strides made in diagnostic recognition, particularly with the inclusion of Complex PTSD in the ICD 11 in 2022, which sheds light on the complexities often overlooked in traditional diagnostic frameworks
2.0 What is Psychological Trauma?
When we feel overwhelmed by a situation or event, or like we can’t cope, and feel powerless to do anything about it, it can be considered a traumatic experience. However it only becomes a trauma when the person’s life continues to be impacted by the traumatic experience of the event or situation.
Trauma is the state of a psychological wound that doesn’t heal.

Traumatic events and situations don’t always lead to a traumatic wound. Two people can experience the same event, and only one will develop a trauma.
There are many things that determine who will, and won’t, develop a trauma response. Here are some of them.
- Age – The person’s age at the time of the experience
- Trauma history – The person’s history of traumatic experiences
- Other vulnerabilities – Other pre-existing vulnerabilities
- Other’s responses – The response given to the person after the event
- Support – Whether the person was able to reach out to others for support.
2.1 Trauma examples
We can divide trauma into three broad categories.
2.1.1 Shock trauma
Shock traumas are typically one-off, sudden, severe, terrifying or life threatening events that cause significant physical or psychological distress. These are the traumas that meet the qualifying criteria for a diagnosis of PTSD.
Here a just a few examples.
Violence
- Violent assaults – Individuals who have been assaulted, whether physically or sexually, may experience psychological shock as they grapple with the trauma and aftermath of the attack.
- Witnessing violence – Observing a violent crime, such as a shooting or assault, can cause intense psychological shock.
Death
- Sudden Loss of Loved One – Experiencing the unexpected death of a close family member or friend can lead to profound shock and grief.
- Near-Death Experiences – Surviving incidents where death was imminent, such as drowning, suffocation, or cardiac arrest, which can lead to profound psychological trauma.

Medical
- Survivors of accidents – People who survive serious accidents, such as car crashes or industrial accidents, may experience psychological shock as they come to terms with the sudden and often life-altering event.
- Medical Emergencies – Enduring sudden and life-threatening medical events like heart attacks, strokes, or severe allergic reactions, which require immediate intervention and may lead to long-term health complications.
Natural world
- Natural disasters – Enduring the devastation of natural disasters, such as bushfires, cyclones, or floods, may cause psychological shock due to the sudden upheaval and loss.
- Animal Attacks – Surviving attacks from aggressive animals, such as dog bites, can cause severe physical injuries and emotional trauma.
Occupational
- First Responders – Emergency responders, such as firefighters, police officers, and paramedics, may experience psychological shock after witnessing or responding to traumatic incidents in the line of duty.
- Military combat veterans – Soldiers who have experienced combat situations, including exposure to enemy fire or witnessing casualties, can suffer from psychological shock as a result of their wartime experiences.
Criminal
- Terrorist attacks – Those who survive terrorist attacks, such as bombings or mass shootings, may experience psychological shock due to the sudden and traumatic nature of the event.
- Hostage Survivors –Those who have been held captive or taken hostage may experience psychological shock due to the trauma and fear they endured during the ordeal.

2.1.2 Relational traumas
Relational traumas typically aren’t as severe or life threatening (though they can be) as shock traumas. These are the traumas that can result in Complex Trauma and can now be recognised by a diagnosis of CPTSD.
There are three elements that make them deeply traumatic:
- Duration – They persist over a long time.
- Repetition – They are repeated, so cumulatively they all add up. The saying ‘death by a thousand cuts’ is another way of describing relational traumas.
- Interpersonal – They occur within relationships, so there is the added element of betrayal trauma. The person has to sort through the minefield of psychological issues that occur when someone who loves them also betrays them by harming them in some way.
Here are some examples.
Childhood trauma
- Neglectful or absent parenting – Growing up in an environment where your parents consistently fail to meet your emotional or physical needs.
- Parental rejection of your gender identity – Experiencing your parents, and/or others, refusing to accept and embrace your gender identity.
- Parental rejection of your sexuality – Growing up with parents, and/or others, who do not accept or embrace your sexuality.
- Parental substance abuse – Living with parents who struggle with addiction, resulting in instability, neglect, or exposure to harmful behaviors.
- Chronic family conflict – Being raised in an environment that has ongoing arguments, tension, or unresolved issues among family members.
- Long-term effects of parents separation – Experiencing the ongoing impacts of parental separation, such as custody battles, parental conflict, or financial strain.
- Parent/child role reversal – Assuming the responsibility of caring for a parent or sibling due to their chronic illness, mental health issues, substance abuse problems or lack of ability.
- Emotional neglect – Growing up in an environment where your emotional needs were consistently disregarded or invalidated.
- Long-term effects of trauma – Suffering from the enduring consequences of childhood trauma, such as abuse, neglect, or witnessing domestic violence.
Adult relationships
- Toxic relationships – Enduring emotional, verbal, or physical abuse from a partner or family member over a prolonged period.
- Rejection of gender your identity – Experiencing other signficiant adults in your life refuse to accept and embrace your gender identity.
- Rejection of your sexuality – Coping with people who are signficant to you refuse to accept or embrace your sexuality.
Peers
- Persistent bullying – Enduring repeated harassment, intimidation, or exclusion from peers over an extended period, leading to social and emotional difficulties.
- Persistent peer rejection – Facing ongoing rejection or social isolation from peers, which can impact self-esteem and social development.
2.1.3 Other experiences
These traumas can also lead to Complex Trauma or CPTSD even though they don’t necessarily occur within relationships. Below are some examples.
- Chronic toxic stress – Prolonged exposure to adversity can lead to lasting psychological impacts such as anxiety and depression.
- Childhood medical procedures – Traumatic medical experiences during childhood can contribute to long-term emotional distress
- Adverse community environments – Growing up in environments characterised by poverty, violence, or instability can have profound psychological effects on individuals.
- Intergenerational trauma -Trauma passed down through generations can result in ongoing emotional challenges and relational difficulties for affected individuals.
You can read more about an alternative way of categorising trauma –Big ‘T’ traumas and small ‘t’ traumas – here.
Next I’ll explain the diagnostic category of Complex PTSD, a significant advancement in recognising the nuanced experiences of trauma survivors, particularly those who have endured prolonged and relational traumas.

3.0 Complex PTSD
Complex PTSD was introduced in the ICD 11, to address the issues of PTSD criteria mentioned above. However as yet, Complex PTSD is not in the DSM 5. Despite this, an increasing number of clinicians are diagnosing people with Complex PTSD, even though they use the DSM 5 as their primary manual.
3.1 Complex PTSD Symptoms
*Note, I have re-worded the criteria for ease of understanding. The following are not to be used for diagnostic purposes.
- PTSD – You must first meet criteria for a diagnosis of PTSD.
- Exposure to Prolonged Trauma – Exposure to an event, or series of events of an extremely threatening or horrific nature, which are most often prolonged or repetitive, and where escape is difficult or impossible. Such events are typically in the context of interpersonal relationships or captivity and include, but are not limited to – prolonged family violence, repeated childhood sexual or physical abuse, torture, slavery, genocide campaigns.

In addition, you must:
- Difficulties regulating emotion – Have severe and persistent problems with emotion regulation. Examples include heightened emotional responses to minor stressors, violent outbursts, reckless or self-destructive behaviour, dissociative symptoms when under stress, feeling emotionally numb -particularly in relation to experiencing pleasure or positive emotions.
- Negative self beliefs – Have beliefs about yourself where you are diminished, defeated or worthless, which are accompanied by feelings of shame, guilt or failure related to the traumatic event. For example, you might feel guilty about not having escaped from, surrendering or being overcome by the traumatic circumstance, or not being able to prevent the suffering of others.
The symptoms must cause significant problems with personal, family, social, educational, occupational functioning. If functioning is maintained, it’s only through significant effort.
3.2 Issues with Complex PTSD Diagnosis
- Qualifying criteria is too narrow – Although Complex PTSD represents progress in acknowledging cumulative trauma, it still excludes some people due to its requirement of “exposure to an event, or series of events of an extremely threatening or horrific nature”. Many people have symptoms consistent with Complex PTSD, but they may not perceive their experiences as meeting the threshold of being “extremely threatening or horrific” events.
- Does not fully encapsulate the depth and breadth of Complex PTSD – There is much more depth and breadth to complex trauma than Complex PTSD covers.
- Not all complex trauma survivors have PTSD symptoms – A diagnosis of Complex PTSD, first requires that the criteria for standard PTSD is met. However, many people who have suffered the most severe complex trauma do not have the core PTSD symptoms (Schwarx, Corrigan et al., 2017, in Blue Knot Foundation, 2019).
PTSD acknowledges the profound impact of intense fear, helplessness, and horror. Complex PTSD acknowledges the added challenges related to emotional regulation, shattered trust in others, and the disruption of self-perception and secure attachment.
Now, I will circle back to the focus of this guide. According to Bessel van der Kolk (2009), complex trauma represents one of the most prevalent sets of psychological issues prompting people to seek therapy. The extensive scope of complex trauma necessitates a diagnosis that comprehensively encapsulates its breadth.
4.0 Complex trauma
“Just as ‘there is more to trauma than PTSD (Shapiro, 2010: 11),
so there is more to complex trauma than Complex PTSD.”
Blue Knot Foundation (2019).
4.1 What is complex trauma?
Complex trauma is the repetition of many traumatic experiences over an extended period of time that have no clear beginning or end. The impact of many traumas, day after day, is emotionally overwhelming, and gradually builds over time, so that the combined impact is huge. The trauma is typically part of the person’s everyday life, it’s in the air that they breathe, and it’s not necessarily life threatening. Finally (though not always) it often occurs within relationships.

4.1.2 Examples of complex trauma causes
Childhood trauma
- Chronic physical, sexual or emotional abuse in childhood
- Ongoing physical or emotional neglect during childhood
- Chronic rejection of your gender identity or sexuality
- Parentification (when a child is forced to take on the role and responsibilities of a parent)
- Domestic physical, sexual or emotional abuse as an adult
- Severe bullying, including cyberbullying, harassment or torture
- Parent or caregiver instability due to mental illness or substance abuse
- Witnessing physical or emotional abuse between parents or caregivers
- Being subjected to forced adoption as a child
Other
- Ongoing discrimination or prejudice, e.g.,.,.,., racial, cultural, homophobia, transphobia, gendered
- Being subjected to forced adoption as an adult (having your baby forcibly removed)
- Witnessing or being a victim of community violence or war
- Being forced or manipulated into prostitution
- Kidnapping, human trafficking, or forced labour
- Being a prisoner of war
4.1.3 Features of complex trauma causes
- Within relationships – It usually occurs between people, where the perpetrator(s) are family members, close friends or in a position of authority
- Repeated – It can occur when you experience repeated trauma as a child, young person or adult
- Trapped– It often involves ‘being or feeling’ trapped
- Intensity – It is often planned, extreme, ongoing and/or repeated
- Enduring impacts – It often has impacts which can last a long time
- Shame – It can cause you to feel ashamed
- Issues with safety and trust– It can stop you feeling safe and being able to trust
- Negative self-feelings – It can make you feel bad about yourself
- Difficulties emotionally regulating – It can make it hard for you to manage your feelings
- Addictions and self harm – It can mean that you use different coping strategies such as alcohol and drugs, self-harm, over- or under-eating or over-working
- Deeply affecting – It can affect your physical and mental health and your wellbeing
- Impacts relationships and family life – It can affect your relationships and your ability to manage your daily life.
4.1.4 Many forms of complex trauma are interpersonal and relational
Many forms of complex trauma occur within the context of a relationship -whether that’s with someone considered close, or someone who is in a position of authority over you. When complex trauma is caused by people in authority, even if they aren’t considered a close relationship, it is deeply impacting. We expect humans to act with a certain level and care regarding other people, and when this does not happen it can leave questioning our own worth and/or trust in humanity.
In close relationships -like a parent/child relationship – we expect a parent to care and protect us. If this care and protection is violated in some way, it can have profound impacts on a person and their relationships with other people -often lasting a lifetime if left untreated. Betrayal trauma describes the added layer of trauma that survivors are burdened by, when someone who should care, does the opposite.
Complex trauma, especially if interpersonally generated,
is well documented to have more extensive impacts
than ‘one-off’, ‘out of the blue’ events.
Blue Knot Foundation (2019).
5.0 Betrayal Trauma
‘Betrayal trauma’ (the term coined by Jennifer Shreyd) describes the deeply traumatising effects of trauma caused by those who should care and protect us. When those who care for us are also abusers, the impacts can be devastating, especially when the victims are children. Shengold has labeled it ‘soul murder’ others have described it as ‘wounds of the soul and spirit’. In cases of complex trauma, maintaining a caring relationship can be crucial. This complexity is especially evident in the context of attachment and survival.
5.1 Attachment ensures survival
5.1.2 Babies and children
Infants and children are biologically programmed to attach to their parents so that they survive. They have certain features, and exhibit a whole host of behaviours to make sure their parents stay around. Think about those gorgeous eyes that are too big for their face, those devine smiles, their cute gurgles and their crying. That’s all designed to keep their parents in love with them and close by. Babies are completely dependent on us. If they don’t have a parent or someone to care for them, they will die. As you can see, attachment seeking behaviours are crucial.
What is Attachment?
Attachment, as described in attachment theory (John Bowlby, 1950s), is the deep emotional bond that forms between a baby and their caregiver.
There are different types of attachment styles, including secure attachment and various forms of insecure attachment (ambivalent, avoidant, and disorganised). These styles result from the caregiver’s responsiveness and sensitivity to the baby’s needs and can have lasting effects on a person’s relationships and emotional well-being throughout life.
5.1.2 Adults and trauma bonds
However, attachment-seeking behaviors do not cease when we grow up. For adults who did not have all their emotional and/or physical needs met in childhood, we often try to fulfill these unmet needs through adult relationships.

5.2 Why do children stay attached to their abusers?
According to Betrayal Trauma theory, children need to stay attached to their parents for survival. So, many children remain blind to the betrayal. If they fully recognised the impact of abuse, they might withdraw from their parent, risking further harm if the parent stopped providing protection and basic needs. Consequently, the child may cope by disconnecting from the impact of the abuse or forgetting it all together.
So, children often remain attached to their abusers as a survival mechanism, which requires blindness to the betrayal in order to maintain the crucial bond they have with their parents.
5.3 What if the carer is also a source of danger?
5.4 Dissociation as a coping mechanism
According to Janina Fisher (2017), the part of us that handles everyday life needs to separate (or dissociate) from the trauma part to avoid feeling overwhelmed. This separation, or dissociation, is a coping mechanism that lets people go about their daily activities despite having traumatic memories and emotions. By compartmentalising these experiences, individuals can manage their responsibilities and enjoy normal activities without being constantly bombarded by distressing thoughts and feelings. This division is essential for keeping a sense of normalcy and preventing trauma from taking over their entire life.
Seeing dissociation as a coping mechanism helps us understand how the mind deals with traumatic experiences by keeping them compartmentalised.

5.5 Repressed memories of trauma
Repressed memories are real. Often, when a traumatic even occurs in childhood, the brain separates out the different elements of the memory into different parts of the brain
- The narrative of the event
- The information the five senses received
- The feeling state of the person at the time of the event
Later in life, the person often has only one of these fragments of memory. But here’s the catch, they don’t realise it’s a memory fragment, because without the other two components of the memory they don’t make sense. We need all three elements to feel like the memory is real.
Here are some examples of memory fragments. This list is far from exhaustive, there are an endless list of memory fragment examples.
- A sense of knowing or suspecting something happened, but having no concrete memory of it
- An unexplained aversion to something, like a smell or a room in a house. The aversion is highly emotional, rather than a simple dislike.
- Intense anxiety with something in particular, that can’t be explained -even if that anxiety is completely unrelated to the actual event.
- A physical sensation that can’t be explained medically. Like a pain at the mention of something.
5.6 Recovered memories
When someone is in therapy, or perhaps they’ve been triggered by something in their life, two of these memory elements may be remembered, or reassociate. The will start to feel like they have discovered a new memory, or ‘recovered a memory’. But, really the memories have been there all along, just disconnected in different parts of the brain.
The popular belief, is that recovered memories are completely new and whole memories of an event. But in reality, it’s putting together -or reassociating- pieces of memory that have always been there and somewhat conscious. Memories are never completely lost, they are there, just separated in different parts of the brain (Pease Banitt, 2018).
Supportive responses from those around us can mitigate the need to repress memories of the abuse. As explored in the following section on how supportive interventions can alleviate the long-term effects of traumatic experiences.
The nature of recovered memories sheds light on how supportive responses can mitigate the impact of trauma, as explored in the following section on how supportive interventions can alleviate the long-term effects of traumatic experiences.
6.0 Supportive Responses can Lessen the Impact of Trauma
There’s one thing that can the impact the severity of your trauma response, or even determine if you go on to develop a long term trauma response – and that’s the support you did, or did not, receive afterwards. Here’s an analogy given to me by a very talented clinician.
“If you broke your arm ten years ago and it still aches today, you’re not in pain because it’s still broken, you’re in pain because it wasn’t set properly and allowed to heal.”
“You’re not in pain just because of the trauma, you’re also in pain
because the trauma wasn’t healed properly.”
Dr Matthew Berry

Long-term trauma responses can be predicted by
- Pre-existing vulnerabilities, like genetics, a highly stressful life.
- The healing we did/did not receive afterwards.
Consider these points
- Who did you tell? What was their reaction? Was your trauma validated or minimised by those around you?
- Were you believed?
- Were you able to seek people out for help after your trauma? Or had you previously learned to shut down, knowing that you wouldn’t be believed, validated or supported? Or was no-one available?
- A pattern of not sharing things that have happened to us is often pre-existing to the trauma.
- Many people have big traumas that are attended to, but it’s the smaller ones that still impact them. A small cut can cause sepsis if not attended to.
6.1 People have three core needs
- Validation Was your trauma recognised by those around you and validated for the impact it had? Or did you receive responses that minimised the impact? Here are some examples of minimising and invalidating responses ‘Don’t be silly, daddy wouldn’t do that’, ‘That’s just what boys are like, they all do things like that’, ‘You can’t let these things get to you, you need to look at the positive’, ‘At least you…(have your health, have another child, have roof over your head, etc.)’
- Connection Did you feel deeply loved by someone? Did you feel supported, like someone had your back? Did you feel seen or invisible in general? Did someone notice what you were going through? Were you loved and accepted for who you are or was it conditional (e.g.,.,.,., were you only accepted if you got great grades)? Do you feel flawed, or like something is deeply wrong with you?
- Safety Were you able to escape the trauma or protect yourself by fighting back? Did you feel physically safe? Did you feel emotionally safe? Did you feel like you could make decisions and take action freely or would you get punished? Did you feel protected by the adults in your life?
When one or more of these three core needs are not met, the likelihood of a long term trauma response increases. Understanding the critical role of supportive responses in mitigating trauma’s long-term effects sets the stage for exploring strategies for healing from trauma, as discussed in the following section on trauma-specific approaches and their importance in effective treatment
7.0 Healing from Trauma
We can’t change the event but we can change the healing.
Dr Matthew Berry
7.1 The Importance of trauma specific approaches
Effective trauma treatments must go beyond the conscious mind, and what you ‘know’, which is what is explored in talk therapy, Effective treatment must access the subconscious or subcortical regions of the brain. Think about it, your trauma responses don’t come from your thinking mind, they occur rapidly, from beneath the cognitive mind. Therefore, treatment must target this deeper level. Trauma cannot be resolved through just talking, thinking or reasoning; if it could, most people would be able to heal themselves.
7.2 How to find a therapist that can treat trauma – what to look for
I can’t overstate the importance of finding a therapist who specialises in trauma treatment. A lot of time can be wasted with therapy that is not designed to address trauma. Below are some crucial areas that your therapist will know about, if they are using an effective trauma treatment.
- Safety – They will talk about emotional and psychological safety a lot. They will know what typically destabilises trauma clients and will do what they can to prevent that from happening.
- Dissociation – They will know about dissociation and the different forms of dissociation, and will constantly monitor you for dissociative states in session.
- Window of tolerance – They will know how, and will assist you, to stay in your ‘window of tolerance‘. This means you should not get too distressed in therapy, and if by chance you do, the therapist will know how to help you return to safety.
- Strengths – Therapy won’t just focus on your trauma. The therapist will also pay attention to building your strengths and helping you learn how to regulate your emotions and self-soothe.

- Implicit memory – Your therapist will know all about implicit memory and the crucial role it plays in trauma therapy. While they may not use that particular term with you, you may hear them talk about ‘parts’ instead, like ‘what does your child part need?’ or they may use methods that help you access emotions from the past.
- Bodily responses – Therapy will address your thoughts, but also your emotional processing and your body’s physical and sensory responses.
- Trauma focused therapy – They should be able to tell you how trauma focused therapy differs to traditional therapy for other issues.
- Sessions end safely – You should always leave therapy feeling safe – that is, feeling ‘in your body’, in an adult state.
Understanding the critical elements of trauma-focused therapy leads us to explore specific therapeutic approaches tailored to complex trauma, such as Emotion Focused Therapy, as detailed in the following section
8.0 Emotion Focused Therapy and Trauma
Working with someone who has experienced complex trauma requires a different approach to working with other psychological issues. I use Emotion Focused Therapy in combination with teachings from the International Society for the Study of Trauma and Dissociation (ISSTD).

8.1 Avoidance of emotions and painful memories
Avoidance is a key behavior in complex trauma because it helps people avoid painful memories and emotions. However, it also has downsides: it can make people avoid lots of situations that are only vaguely similar to their trauma and stops them from processing and resolving their traumatic experiences.
The first two goals of therapy for complex trauma, is to address both of the core traumas that lead people to rely on avoidance strategies.
8.2 The two core injuries of complex trauma
There are two core wounds that complex trauma survivors have, that lead them to rely on avoidance strategies.
1. Not having the safety and security you needed in your closest relationships
When children have a parent who’s there for them both physically and emotionally, they feel safe and secure. They can go out and explore, knowing their parent will be there if they need help, protecting or comforting. With lots of these experiences, they learn to feel safe inside. So eventually, even when their parent isn’t there physically, they still carry that feeling of safety. For children that don’t have that kind of parent, they don’t get that internal sense of safety. Instead, they internalise a feeling of being on their own, unsafe, and unable to handle things.
2. Not having had the chance, regular role modeling, and coaching to learn how to manage your emotions better.
Securely attached children have parents who demonstrate how to handle emotions. When the baby or child is upset, the parent hugs them, comforts them with soothing words, and remains calm until the child settles. This teaches the child that emotions are safe, manageable and temporary. Through repeated experiences, the child learns to feel safe with their emotions and develops self-soothing skills. When a child doesn’t have these experiences, emotions become terrifying, overwhelming and unending, and are avoided at all costs.

2. Emotion regulation; Overcoming the lack of role modeling and coaching to better manage your emotions
8.4 Trauma processing
When I help people work through their trauma, I use Emotion Focused Therapy and rely heavily on Melissa Harte’s Expanded Focusing Task (Harte, 2019). Melissa’s model stems from Emotion Focused Therapy but is heavily informed by neurobiological research on trauma, ensuring a comprehensive approach that addresses both emotional and physiological aspects of trauma recovery.

8.4.1 Bottom up approach
I use a bottom-up approach in trauma therapy, which is crucial because it directly deals with how trauma gets stored in the body. Traumatic experiences activate the body’s fight, flight, or freeze response, which can stay turned on in survivors, leading to constant alertness, anxiety, and an overactive stress response.
Complex trauma is a common and complex issue that deeply affects a person’s emotional and mental health. There is no official diagnosis for complex trauma, though CPTSD is the closest available. However the symptoms aren’t as specific as those required for a diagnosis of C-PTSD, though they are just as deeply impacting.
When dealing with complex trauma, it’s crucial to get therapy that is designed for complex trauma. Emotion Focused Therapy helps tackle the deep wounds caused by complex trauma by targeting the physical effects of trauma to calm down the body’s nervous system and change traumatic feelings into ones that are easier to deal with. This doesn’t erase the memory of what happened, but it changes how it affects your emotions, leading to more complete and lasting healing.
References
Blue Knot Foundation (2019). Practice Guidelines for Clinical Treatment of Complex Trauma. Authors- Kezelman, C.A.., & Stavropoulos, P. Retrieved from www.blueknot.org.au
Courtois, C. A., & Ford, J. D. (Eds.). (2013). Treating complex trauma in children and adolescents: Scientific foundations and therapeutic models. The Guilford Press.
Courtois, C. A., & Ford, J. D. (2016). Treatment of complex trauma: A sequenced, relationship-based approach. The Guilford Press.
Fisher, J. (2017). Healing the fragmented selves of trauma survivors: Overcoming internal self-alienation. Routledge.
Harte, M. (2019). Processing emotional pain using emotion-focused therapy: A guide to safely working with and resolving emotional injuries and trauma. Australian Academic Press.
Herman, J. L. (1992). Trauma and recovery: The aftermath of violence–from domestic abuse to political terror. Basic Books.
Pease Banitt, S. (2018). Wisdom, attachment, and love in trauma therapy: Beyond evidence-based practice. Routledge.
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Penguin Books.
Take the First Step Towards Healing
If you're struggling with complex trauma, don't face it alone. Contact me today and start your journey to trauma recovery.
Emotion Regulation and Trauma: Why It Feels So Hard to Manage Your Emotions
If you’ve experienced relational trauma, emotion regulation may be something you really struggle with. Emotion regulation is being able to acknowledge and accept your feelings, to make sense of them without becoming overwhelmed or shutting down, and to respond in a...
Self-Worth Part 2 – How Do I Feel Worthy Enough?
It is possible! Feeling worthy enough now, is about knowing that your worth as a human is not tied to anything external, deeply internalising that you are enough, now, simply for being human. This deep knowing can be achieved in various ways. Obviously I am biased and...
Self-Worth Part 1 – Why You’re Already Enough
One therapy goal that comes up consistently with clients, is a wish for better self-esteem, self-worth, or self-love. The thinking seems to be that this quality needs to be gotten somehow, or more of it needs to be obtained, or built in some way. This thinking makes...